At least 170 healthcare practitioners have been equipped with essential skills to address Sexual and Reproductive Health (SRH) needs in crises through a series of formal training sessions conducted across five provinces in Zimbabwe on the Minimum Initial Service Package (MISP) under the Health Resilience Fund programme. The provinces trained so far include Mashonaland West, Mashonaland East, Mashonaland Central, Manicaland, and the Midlands.
The MISP, developed by the Inter-Agency Working Group for Reproductive Health in Crisis (IAWG), outlines a set of lifesaving activities crucial for responding to SRH needs at the onset of humanitarian emergencies. These needs often go unmet, leading to devastating consequences for affected populations.
The package addresses five key objectives of:
- Ensuring health cluster lead for the implementation of MISP
- Prevention of sexual violence and assistance of survivors
- Reduction of HIV transmission
- Prevention of excess maternal and neonatal morbidity and mortality
- Planning for comprehensive RH services integrated into Primary Health Care
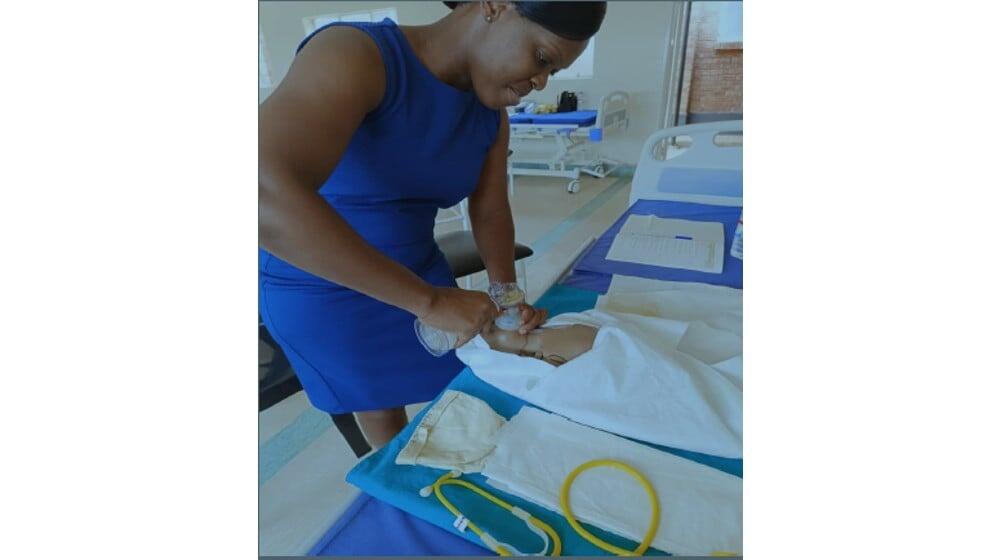
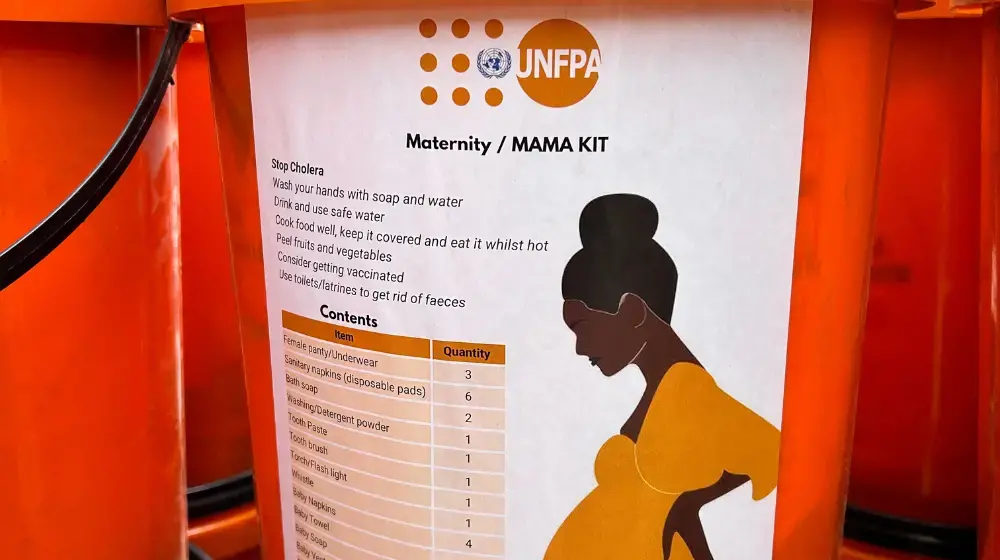
The training aimed to enhance participants' understanding of the MISP and its importance in reducing morbidity and mortality related to SRH. Key objectives included explaining the significance of addressing SRH in emergencies, understanding the services included in the package, exploring emergency reproductive health kits, and examining global and national coordination mechanisms. Additionally, participants reflected on delivering MISP in line with existing policies and identifying stakeholders' roles in improving preparedness.
The training primarily targeted programme managers, the Provincial Health Teams who supervise health/SRHR projects, including health staff with decision-making responsibilities. Participants included Provincial Medical Directors, Maternal, Newborn and Child Health Officers, Reproductive Health Officers, Nurses, Doctors, Pharmacists, Mental Health Officers, Environmental Health Officers, and Nutritionists.
A marked improvement in results was observed between pre- and post-training assessments, demonstrating the effectiveness of the training in enhancing participants' knowledge and skills. The sessions employed a variety of interactive methods, including presentations, group discussions, case studies, role-plays, videos, demonstrations, and participatory activities.
Participants were able to reflect on the humanitarian response they provided to the Covid-19 response and current response to the cholera outbreak. Strengths, weaknesses, challenges were discussed and recommendations for improvement noted.
Following the training, participants were encouraged to develop provincial and district action plans for implementing MISP integrated into their broader plans. There will be follow up on the work plans the provinces will develop. By building capacity among healthcare practitioners, the MISP training initiative represents a significant step forward in Zimbabwe's efforts to protect the sexual and reproductive health of its population during crises.
The Health Resilience Fund is a coordinated effort by the Government of Zimbabwe and Development Partners in support of the Ministry of Health and Child Care, to improve health systems resilience to shocks, equitable access to quality health care in Zimbabwe, with special emphasis on women, new-borns, children, adolescents, youth, and health emergencies running from 2022 to 2025.
It is led by the Ministry of Health and Child Care with financial contributions from the European Union, the Governments of Ireland and the United Kingdom, and Gavi, the Vaccine Alliance, and technical support from UNFPA, UNICEF, and the WHO.